The learning eventsDoes the NHS have the ability to deliver the level of system-wide change required of it? How can its leaders learn the lessons – the must-dos, and the elephant traps – from past attempts of system change?
Through a series of learning events in May 2018, UCL and Kaleidoscope Health & Care explored the implications of the reconfiguration of stroke services in London and Greater Manchester for system-wide change in the NHS in England. This included new findings from research led by University College London on how to make and sustain major system change. The events shared learning across a wide range of clinical areas and perspectives, helping participants deliver change for the better. The changesBackground
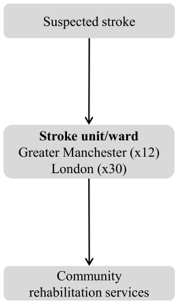
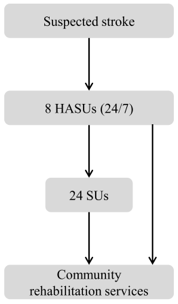
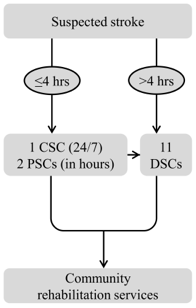
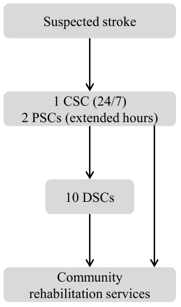
Major health system change involves reorganisation of services, at the regional level, and may include significant alterations to a care pathway. One such change is service centralisation, whereby aspects of service provision across a region are concentrated in a reduced number of hospitals. Significant changes in provision of clinical care in the English NHS have been discussed in recent years, with the proposal to concentrate specialist services in fewer centres serving larger populations. Clear evidence of unacceptable variations in quality of care has prompted radical reorganisation (or ‘reconfiguration’) of stroke services in several regions of England. The changes studied The evaluation of major system change in acute stroke services was funded by the NIHR Health Services and Delivery Research programme, and ran from 2011 to 2017. It focused primarily on the process and impact of centralising hospital stroke services in London and Greater Manchester into specialist hyperacute stroke units. The changes are summarised below. Before the changes: London and Greater Manchester
London centralisation
Greater Manchester initial centralisation - ‘Greater Manchester A’
Further centralisation - ‘Greater Manchester B'
|
The researchThis was a mixed methods evaluation, drawing on combining quantitative methods (analysing what works at what cost) and qualitative methods (analysing factors influencing development, implementation, and sustainability of changes). analysis of “what works and at what cost?” with qualitative analyses of “understanding implementation and sustainability” in order to analyse major system change in acute stroke care in a range of settings across the English NHS.
Our research questions were:
The evaluation was a collaboration between stroke clinicians and academics based in London and Greater Manchester, and actively involved a wide range of other stakeholders, including stroke patients and carers, commissioners, and the voluntary sector. The research team included Chief investigator Professor Naomi Fulop, and co-investigators Professor Anthony Rudd, Professor Pippa Tyrrell, Professor Ruth Boaden, Professor Charles Wolfe, Professor Christopher McKevitt, Professor Steve Morris, Dr Angus Ramsay, and Rachael Hunter. Key findings from this evaluation are summarised below. To date, our published research has been referred to in national policy (Five Year Forward View), clinical recommendations (RCP Stroke Clinical Guideline), and has been cited in several ‘case for change’ documents’, including in Greater Manchester, where further centralisation was implemented in March 2015. |
Key findingsWhat works at what cost:
Development, implementation, and sustainability
Italicised findings are as yet unpublished. |